The Psychiatric Cost of Medically Assisted Death — MAID

This essay was written by Hannah Spier, MD, author of PsychobabbleWithSpier. She is a Psychiatrist in the Netherlands, which alongside Canada, allows patients to chose euthanasia in cases of depression, anorexia and other mental health problems.
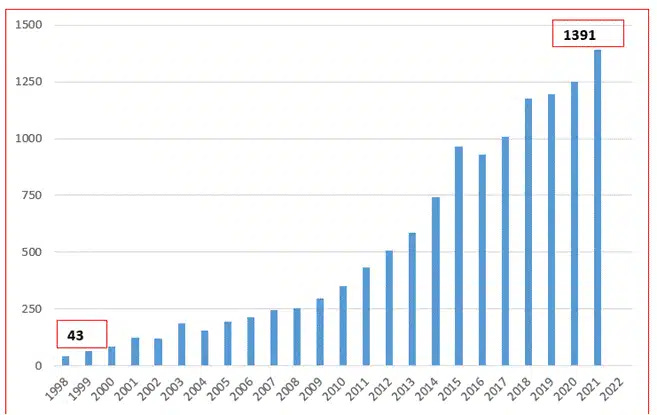
In 2024, the Netherlands reported a record 219 people killed through state-sanctioned euthanasia for psychological suffering—mostly depression—marking a 60% increase from the year before. In Switzerland, where “self-determined death” is practically a civic virtue, over 1,200 people ended their lives with the help of assisted suicide groups in 2023. This same year, Canada caught up by providing medically assisted death (MAiD) to 15,343 patients. However, they just postponed the expansion of MAiD to people with mental illness until 2027, after widespread backlash. Perhaps fuelled by the unsettling frequency of stories involving patients being offered MAiD against their wishes.
It’s sure to be only a delay. The trend has been steady for over a decade. This has been driven by overzealous professionals and bureaucrats with a progressive worldview, having reduced the meaning of life to the virtues they hold highest: choice, dignity, and autonomy. These values, once secondary to healing, now form the primary ethical framework. The message, repackaged as empowerment, is clear: if your life lacks these virtues, it’s not worth enduring.
THE NEW ETHICS OF DEATH
This is not just a philosophical shift. But rather, it's an existential collapse of the psychiatric profession. Because once we accept that some lives are not worth living, we are forced to ask: what now is the role of psychiatry? Are we to redefine the criteria of mental illness to allow for a process in which we calmly tell a suicidal patient, “Yes, perhaps you're right”?
Historically, suicidal ideation was a sentinel symptom of mental illness. During residency, it was drilled into us: identifying and preventing suicide is your most important task. Miss it, and you’ve failed. The suicidal mind is not rational, but consumed by pain. It is unable to see beyond the present moment. Depression narrows your field of vision. So, our task is to help patients see beyond the blackness and believe in the possibility of light.
Our job is to hold the hope our patients cannot.

One technique that stayed with me: when someone talks about jumping in front of a train, you ask them to imagine the conductor. Will he recover? Will he be able to work again? Feed his children? Sometimes it’s not dignity or autonomy that keeps people alive, it’s empathy and connection. It’s love for those we would leave behind.
Yet today, duty to others is framed as emotional manipulation. “Why should I live for others?” becomes the mantra of a hyper-individualist culture. Stoicism is recast as repression. Dignity is reduced to self-sufficiency. To need help is to lose worth.
I once treated a man who was asked to be the person present at his friend’s assisted suicide appointment through EXIT in Switzerland. He had no psychiatric history. But after four postponed death dates, he was suffering from anxiety and insomnia. He couldn’t express his discomfort for fear of seeming “unfeeling.” So, he suffered in silence. Alone. For months. That’s the quiet trauma rarely discussed, covered up by the sanitized language of “death with dignity.”
THE CLINICAL CONSEQUENCES
Meanwhile, we’re told depression is treatable. And it often is. But treatment begins with a commitment to life. The new ethos, now written into law, says: maybe you’re right, maybe your life is indeed unbearable.
This leads to a profound contradiction. Since psychiatry has long fought to reduce stigma by insisting psychological suffering is equal to physical pain, we can no longer meaningfully distinguish between physical and mental illness. If MAiD exists to spare people from suffering, logic demands we don’t deny it to those whose pain is mental. The moment we accept MAiD for physical illness; we’ve already justified it for psychiatric conditions.

But then come the implications. Suicidal ideation used to mark clinical depression. So, what are we to make of all these patients requesting death? Are they mentally ill and therefore unfit to consent—or mentally sound and therefore not disordered? Do we now divide suicidality into two types: rational and irrational? At what point do I, as a clinician, say to a patient: You aren’t depressed. You’re just realistic.?
This isn’t theoretical. Psychiatry is already struggling with diagnostic ambiguity. A well-known study comparing British and American psychiatrists found they gave wildly different diagnoses for the same kind of patient. And yet we’re meant to determine—confidently—which patients are of “sound mind” and suffering from “chronic, untreatable suicidality”? Based on what?
In a field built on subjectivity, how can we abrogate the authority to decide which suicides are tragic and which are rational?
And what does that mean for the rest of our patients? For years, our role was to guard the flicker of hope, to widen the patient’s perspective beyond the walls their illness had built. If we tell some patients their suffering is too great to bear, what message does that send to the others who are still trying?
WHEN CHOICE BECOMES PRESSURE
This isn’t just a psychiatric dilemma—it’s cultural. When I became a full-time mother, strangers lamented my “wasted education.” I was “not contributing.” That same utilitarian ethic now shadows the elderly and mentally ill: if you're not productive or autonomous, you're perceived as a burden.
Once a society offers assisted suicide as a dignified option for some, the mere existence of that “choice” exerts pressure on others. It quietly redefines which lives are worth living and which are not. What begins as autonomy for one becomes coercion for another.
On the website of EXIT, one of the Swiss MAiD organizations, they reassure families that scheduled deaths make mourning “easier.” Imagine lying in a hospital bed, suffering the same illness as the person beside you, and overhearing: “It’s probably for the best. Your family gets to say goodbye properly.” You can’t help but wonder: How am I different? The next time your family visits, what will you imagine seeing in their eyes?
Then there’s the quite common issue of patients signing the MAiD papers, and changing their minds later. Imagine I tell a patient: “Yes, your suicide is rational. I agree with you.” They come back days or weeks later, having changed their mind. They ask for help. What do I say then? Can I still offer hope for tomorrow, after already affirming that their suffering was beyond hope? Can I deter the suicide with encouraging thought and empathy for those left behind? Especially when we have already recast such connection repressive emotional manipulation at the expense of the sufferer?
Once we legitimize suicidality by approving MAiD, we have, in effect, declared that there is no path forward, how do we walk it with them after that? Assuming there is still a trustworthy therapeutic relationship after all these lies.
Even the most reluctant supporters of MAiD—those who cautiously make allowances for the “truly hopeless” terminal cases—fail to see the larger picture. They don’t sit where I sit, where the rubber hits the road. They fail to acknowledge the ripple effects unleashed by the moral framework that makes MAiD acceptable in the first place.
The framework that shifted away from the belief in intrinsic human value and reduced human worth to the dignity of being independent and productive in the absence of suffering.
But amid a mental health crisis afflicting every Western country, how can we possibly justify sending teenagers the message that the value of life is conditional, and that death is just another lifestyle choice?
I’m tasked with fighting a suicide epidemic while the only tools I have available are being stripped from my hands. I’m expected to instil hope, while the law quietly affirms despair as a valid endpoint. It's like trying to talk someone off a ledge while the crowd below is cheering them on for jumping.
Follow Dr. Hannah Spier at PsychobabbleWithSpier. She describes herself as "The Antifeminist Psychiatrist" and aims to expose "bad therapy and and the liberal narratives that contribute to our poor health." You can keep up with her writings on X: @hannahspierMD.